How Did the Measles Outbreak in Texas Start? Tracing the Roots of a Public Health Crisis
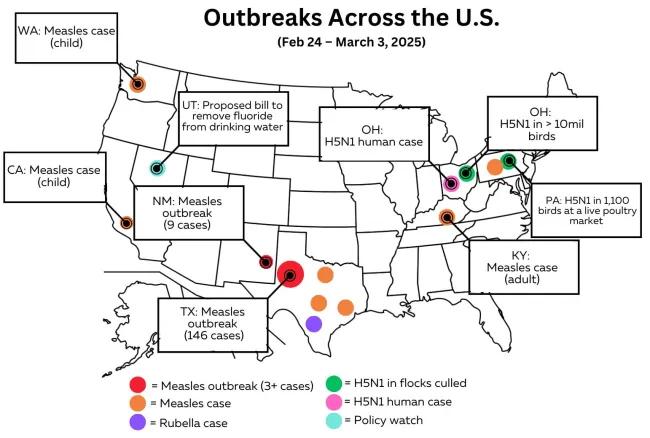
The measles outbreak currently sweeping through Texas has become the state's worst in decades, with hundreds of confirmed cases and multiple tragic deaths. This preventable disease has resurged in communities where vaccination rates have fallen dangerously low. Let's examine how this outbreak began and what factors allowed it to spread so rapidly.
The Initial Spark: Patient Zero and Early Spread
The outbreak appears to have started in late January 2025 in rural West Texas, particularly affecting a close-knit religious community with historically low vaccination rates. Measles, which was declared eliminated in the U.S. over two decades ago, found the perfect conditions to take hold:
- The first cases were likely linked to international travel, as measles remains common in many parts of the world
- The virus spread quickly through unvaccinated households, schools, and community gatherings
- Within weeks, what began as a localized outbreak expanded across county lines
Why Texas? Key Factors Behind the Outbreak
1. Declining Vaccination Rates
Texas has seen a steady increase in vaccine exemptions over the past decade. Many parents now opt out of school-required immunizations for non-medical reasons, creating pockets of vulnerable populations.
2. Lingering Misinformation
False claims about vaccine safety, some dating back to long-debunked studies, continue to circulate. The COVID-19 pandemic further eroded trust in public health recommendations among some communities.
3. Unique Community Factors
The outbreak initially spread fastest in tight-knit groups that tend to homeschool and have limited engagement with public health systems. Similar patterns have been seen in previous measles outbreaks across the country.
4. Public Health Challenges
Texas laws limit local health authorities' ability to mandate vaccines or quarantine measures. Rural areas often lack the healthcare infrastructure needed for rapid outbreak response.
The Outbreak Expands
What began as a localized problem soon became a multi-county crisis:
- Cases appeared in neighboring states, linked to travel from affected Texas communities
- Hospitals reported increasing numbers of severe cases requiring intensive care
- Public health departments scrambled to set up vaccination clinics and containment measures
Lessons From the Crisis
This ongoing outbreak highlights several critical public health issues:
- Herd Immunity Matters - Even small drops in vaccination rates can allow dangerous diseases to resurge
- Misinformation Has Consequences - False claims about vaccines put entire communities at risk
- Preparedness Is Key - Public health systems need adequate funding and flexibility to respond to outbreaks
What Can Be Done?
Health officials emphasize that it's not too late to:
- Get vaccinated if you or your children haven't been
- Check vaccination records and update any missing doses
- Consult trusted medical professionals about vaccine safety
- Support public health efforts to contain the outbreak