GLP-1 Drug Exenatide Fails to Improve Parkinson's Disease Outcomes, Study Finds
A large clinical trial has found that exenatide, a GLP-1 drug, offers no benefit in improving movement, symptoms, or brain imaging in people with Parkinson’s disease, despite earlier promising results.
Background
- Parkinson’s Disease and GLP-1 Medications:
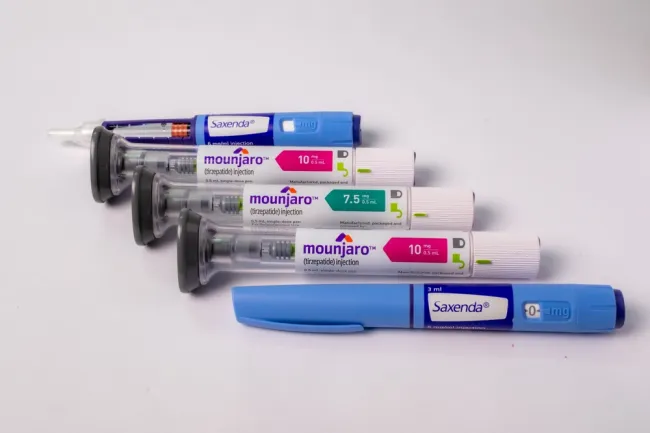
Parkinson’s disease is a degenerative neurological condition that affects movement and other bodily functions. Medications in the GLP-1 class—such as exenatide, semaglutide (Wegovy), and Ozempic—are primarily used to treat Type 2 diabetes and support weight loss, but they have also been studied for potential neuroprotective effects. - Previous Findings:
Smaller initial studies had suggested that exenatide might slow the progression of Parkinson’s disease, prompting a larger trial to confirm these early results.
Study Overview
- Objective:
The study aimed to determine whether exenatide could offer therapeutic benefits or slow the progression of Parkinson’s disease. - Methodology:
In this phase 3, randomized, double-blind controlled trial, participants received weekly injections of either exenatide or an identical-appearing placebo. - Participants and Duration:
The trial enrolled 194 individuals with Parkinson’s disease and was conducted over 96 weeks at six UK hospitals in London, Oxford, Plymouth, Salford, and Edinburgh. - Funding and Support:
The study was funded by the National Institute for Health & Care Research (NIHR) and received additional support from organizations including Cure Parkinson’s and the Van Andel Institute.
Results
- Key Findings:
Researchers found no significant differences between the exenatide and placebo groups in terms of:- Objective measures of movement
- Patient-reported symptom severity
- Brain imaging outcomes
- Adherence Verification:
Blood tests confirmed high adherence among participants, which reinforces the reliability of these negative findings.
Expert Insights
- Professor Thomas Foltynie’s Perspective:
The lead researcher and professor at the UCL Queen Square Institute of Neurology explained that it remains unclear whether any subgroup of Parkinson’s patients might benefit from exenatide. He mentioned that further analysis is planned, particularly to determine if factors such as pre-diabetic blood test results could be associated with a better treatment response—a possibility suggested by earlier studies.
Implementation and Support
- Institutions Involved:
The trial was conducted at the UCL Queen Square Institute of Neurology and the UCLH National Hospital for Neurology and Neurosurgery. - Collaborative Partners:
The study was supported by the UCL Comprehensive Clinical Trials Unit (UCL CCTU), the UCLH Biomedical Research Centre, and the NIHR UCLH Clinical Research Facility.
Implications and Future Directions
- Impact on the Community:
The lack of benefit from exenatide represents a significant setback for both patients and researchers, especially given the promise shown by earlier studies. - Ongoing Research:
Despite these disappointing results, the research team will continue to analyze the data to identify any potential subgroups of patients who might benefit from the treatment. This ongoing effort highlights the need for innovative approaches in developing effective therapies for Parkinson’s disease.
This structured overview has been refined for clarity and flow while maintaining all essential information about the study and its findings.